
Fending off a blood sugar low while on the send
Scenario: The favorite part of your day has finally arrived. You are at the gym standing below a route that crushed you last time instead of the other way around. But with renewed spirit you have regained strength, composure, and found more mental grit to make another attempt. As you stand below the monstrosity visualizing the crux that defeated you, a familiar nervousness shimmers through your body like goosebumps; your fingers begin to tremble, but you ignore it because this is your time to conquer the project. With your eyes transfixed on the route your arms and neck start projecting the movements up the slab.
Crimp rock with the right hand, left foot into the crack, huge slope rocks for the next three movements with an explosive dynamic move to the jug rocks with both hands. Then come the rocks the width of your fingernails that swallowed you whole the last attempt you made, but not today. You have rested as much as your busy lifestyle will allow, hydrated when you remember and refueled properly, except for skipping a few meals here and there. A quick energy bar and glass of milk in the late afternoon will have to suffice you told yourself. Dismissing the thought your body trails onward and upward reaching the final rock.
As the visualization ends your nervousness and shaky hands are accompanied by an increased heart rate and a slightly dizzy feeling. Your forehead and neck have drops of perspiration that were not there after warm-up. A wash of fatigue suddenly grips your legs, spine, neck, and arms. You feel “off” and know something is not right. Your climbing buddy notices a ghostly paleness to your face and suggests sitting down on the crash mats for a bit.
The glazed-over look in your eyes and confused voice have made him realize something is amiss. In the back of your mind you remember the doctor mentioning something about frequently checking your blood glucose with a new machine, and watching for hypo’s (whatever that means…) and carrying around that expensive glucagon shot thing that you can never remember to grab on your way out the door.
But thankfully it’s not a secret and your climbing partner knows you are a newly diagnosed diabetic. He has family members with the condition and has a well-trained eye for signs/symptoms of a hypoglycemic or hyperglycemic episode. Knowing your typical lifestyle and lack of recent compliance to carbohydrate counting and blood glucose monitoring, he knows you need sugar . . . fast. Reacting quickly, he rushes over to the vending machine and gets a packet of gummies and a regular soda. He instructs you to drink half the soda and eat the gummies. Leaving you with another climber he goes in search of your backpack to find the blood glucose monitor you never use. “It’s time to check your sugar levels, brah”, and after another pause says, “all the time.” In the fogginess of the moment, as your head hangs down, all you can muster is, “Dude, I never even made it on the wall.”
Defeat. Setback. Failure. If you have ever experienced a hypoglycemic episode during an exercise session these thoughts and feelings may seem familiar to you.
Ways to manage a low blood sugar episode
Know how to implement the Rule of 15 when hypoglycemic symptoms occur.
AS SOON AS SYMPTOMS APPEAR:
1: If possible, check blood glucose.
2: Eat/drink 15 grams of fast acting carbohydrate wait 15 minutes.
3: Recheck blood glucose, if below 70 mg/dl eat another 15 grams of fast acting carbohydrate and wait 15 minutes.
4: Recheck blood glucose, if below 70 mg/dl, call 911.

What foods have 15 grams of fast-acting carbohydrate?
- 3-4 glucose tablets
- 4-6 oz juice
- 4-6 oz regular soda
- Fun size packet of Skittles
- 4 Starburst
- 1 packet fruit snacks or gummies
- 1 small box of raisins
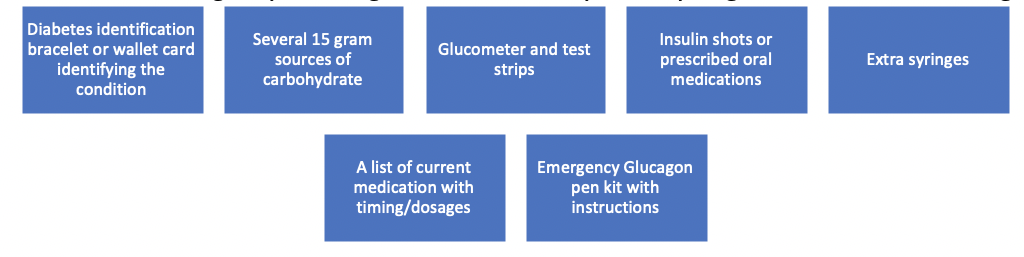
Make a diabetes emergency “Go Bag”
Take it everywhere you go. Include the following:
According to the American Diabetes Association, there are over 1.4 million new cases of diabetes each year (3). If you happen to be newly diagnosed it is imperative to seek counseling from a registered dietitian (RD) or certified diabetes educator (CDCES); treatment is individually based. Every diabetic has unique blood glucose patterns and a RD/CDE will be able to recommend the correct total daily dose of insulin, configure your insulin sensitivity factor, structure meal plans with adequate carbohydrate to fuel your exercise regimen, and educate you on the signs and symptoms of hypo/hyperglycemia.
Taking steps to properly care for yourself can be lifesaving and get you back to crushing projects in no time at all. Long gone will be the days when becoming weak in the knees from looking up at the crag is caused by low blood sugar, next time it will be because the challenge ahead is daunting and intimidating.
We all know how the story ends for the motivated climber, the rush of adrenaline kicks in and the call to, “climb on” rings tried and true. However, this time the equipment to traverse is not just the rope, harness, chalk bag, and carabiner; it includes your “Go Bag” too.
Works Cited:
- Brooks, M. (2016). Blood glucose monitoring. [Powerpoint slides].Retrieved from https://mediacast.ttu.edu/Mediasite/Play/decf596f0b2748b8ae5f750848e1da791d
- Brooks, M. (2016). Acute complications. [Powerpoint slides]. Retrieved from https://mediacast.ttu.edu/Mediasite/Play/ff4cdf0ec3724bd48ce0ba88de248ec11d
- Brooks, M. (2016). Disease process and macronutrient metabolism. [Powerpoint slides]. Retrieved from https://mediacast.ttu.edu/Mediasite/Play/71bee02b44e246c7a12bd98b34ab0e4b1d
Written by Lindsay Opie RD, LD
~This is general information only and not medical advice. Always consult with your healthcare professional before undergoing any diet, medication, or lifestyle change.
Want to learn more? Check out our on-demand masterclass Nutrition for Climbers, or our book Nutrition for Climbers: Fuel for the Send.
